Neuropathic Pain: A Glimpse Inside the Unabating Affliction
MARCH 20, 2018 Jerry A. Barbee Jr, PharmD, CPh; Matthew Savoie, PharmD; Catherine M. Kew, PharmD Candidate; and Alexis Smith, PharmD Candidate
A study published recently in the Journal of Pain Research reported the prevalence of neuropathic pain at 10% in the US population.1 The National Institute of Neurological Disorders and Stroke (NINDS) reported that 20 million Americans have some type of peripheral neuropathy.2 Neuropathic pain is defined as “pain caused by a lesion or disease of the somatosensory nervous system.”3 Although nociceptive pain results from nociceptor response to tissue injury, neuropathic pain occurs as a consequence of nociceptor damage. Originating from damage within nerve cells themselves, neuropathic pain is often complex, with many treatment challenges. Because of its numerous etiologies and minimal response to opioids, careful evaluation and multimodal treatment should be anticipated in managing neuropathy.
OVERVIEW OF NEUROPATHIC PAIN
Neuropathic pain is associated with many symptoms and classifications. With more than 100 types of neuropathy recorded, each case is unique.2 Those with neuropathic pain can present with mononeuropathy or polyneuropathy of axonal or myelin origin.2 Axonal refers to pain originating from axonal damage, while myelin origin results from demyelination of a nerve cell myelin sheath. Neuropathies may occur secondary to damage of either origin or a combination of both axonal and myelin. Mononeuropathy is when an individual incurs damage to a single nerve (eg, carpal tunnel), and polyneuropathy is a “diffuse peripheral nerve disorder that is not confined to the distribution of a single nerve or a single limb.”4 Polyneuropathies typically present as symmetrical and bilateral, with sensory loss, weakness, or burning.5
Neuropathic pain generally occurs as chronic pain that escalates. However, neuropathy can be acute or chronic. Chronic manifestations commence with subtle pain and develop gradually. By contrast, pain in an acute form develops spontaneously, advances quickly, and resolves slowly as the injured nerve cells begin to heal.2 Guillain-Barr syndrome, a commonly known acute neuropathy, results from an individual’s immune system attacking its own peripheral nerves. Unlike chronic neuropathic pain, this syndrome typically lasts a few weeks, with most patients suffering no long-term complications.6
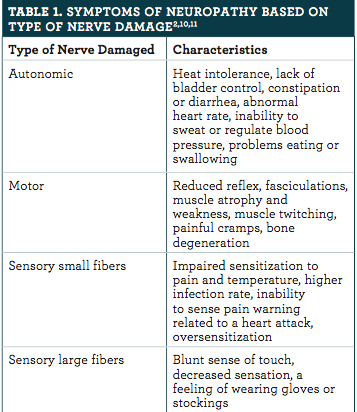
General manifestations of neuropathy include allodynia, anesthesia dolorosa, hyperalgesia, and hyperpathia.7,8 However, symptoms of neuropathic pain can vary greatly, depending on the type of nerve that is damaged. Autonomic, motor, and sensory nerve damage each have unique characteristics, which may help identify an underlying origin (online table 1).2,9,10
Symptoms can also be classified as negative or positive based on their physiological effect. Negative symptoms, including the loss of sensation and numbness, are common in diabetic neuropathy and are a major contributing factor to the high rate of amputations in patients with diabetes. Positive symptoms include increased pain sensation, spontaneous pain, and paresthesia (burning or prickling sensations).11
Most often, nerve damage results in chronic symptoms that resolve only if the cause is recognized and can be rectified. However, symptoms may persist, despite treating the underlying cause, because of changes in the central nervous system (CNS).8
ETIOLOGY
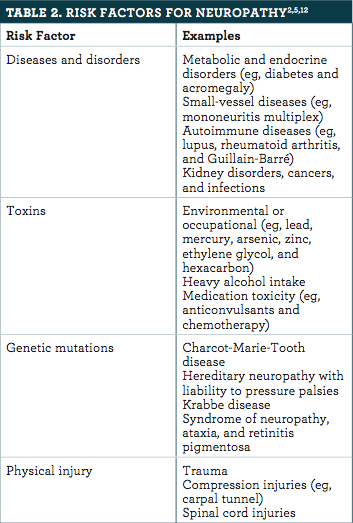
NINDS has identified 4 main causes (or risk factors) that are associated with neuropathic pain. These are diseases and disorders, exposure to toxins, genetic mutations, and physical injury (online table 2).2,5,12 The 4 categories show the diversity of neuropathic pain etiologies and explain why neuropathic pain can be difficult to treat. Peripheral neuropathy is most often associated with diabetic neuropathy, as well as neuropathic cancer pain, postherpetic neuralgia, and trigeminal neuralgia.7 Central neuropathy is often correlated to multiple sclerosis, a spinal cord injury, or a stroke.7
PATHOGENESIS
The transmission of pain involves complex signaling pathways and numerous endogenous neurotrans- mitters (NTs), including calcium, gamma aminobutyric acid (GABA), glutamate, potassium, and sodium.11 Glutamate is the major excitatory NT with the ability to increase pain, and GABA is the major inhibitory NT that decreases pain. In the nociceptive pain pathway, nociceptors are stimulated, leading to a process called transduction in which the activation of nociceptors converts the stimuli to electrical activity. Then, through transmission and modulation, the electrical message is sent and potentially altered as it travels through the nervous system (dorsal root ganglion, spinothalamic tract, thalamus). Once the stimulus reaches the higher cortical structure, the somatosensory cortex, perception occurs and the stimulus becomes a conscious pain experience. However, in neuropathic pain, a direct stimulus is not involved and dysfunctional nerves lead to unnecessary generation of pain.
Unlike nociceptive pain, neuropathic pain is most often classified as chronic pain, which may increase in intensity over time. Although the mechanisms behind neuropathic pain are not completely understood, several mechanisms that influence the peripheral nervous system (PNS) and CNS have been identified. Three primary mechanisms that may be responsible for PNS neuropathy include unprompted firing of damaged nerves, increased sensitivity of the afferent pathways because of denervation (the loss of nerve supply), and sympathetically sustained pain.13 By contrast, neuropathic pain of CNS origin may result from sensitization at the synapses or restructuring of higher-processing operations.13
DIAGNOSIS
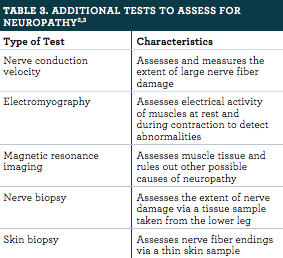
Neuropathic pain is usually suspected based on the presence of symptoms.7,8 As mentioned, patients can present with varying signs and symptoms depending on the mechanism causing the neuropathy, but the underlying cause may or may not be apparent.7 A clinical examination is necessary for a diagnosis of neuropathic pain.3 Patients undergo neurological examination, with a review of their medical history.2 A physical exam and sensory testing are performed to assess muscle strength and the ability to detect light touch, temperature, body position, and pain.2,3 Additional tests, which are outlined in online table 3, may be conducted.2,3
TREATMENT
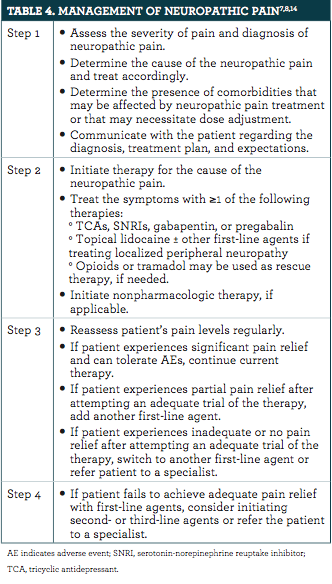
The management of neuropathic pain is typically a multimodal process (online table 4).7,8,14 Treatment plans should be discussed with patients and include the reason why pharmacologic therapy is being selected, the benefits and adverse events (AEs) of therapy, the dose titration schedule, how to manage AEs, and nonpharmacologic therapies.14 Patients should be referred to a pain specialist or a specialist in the underlying condition if their pain is severe or significantly debilitating or if the underlying condition worsens.14
Pharmacological agents used to manage neuropathy are outlined in online table 5 and online table 6.3,8,14-16
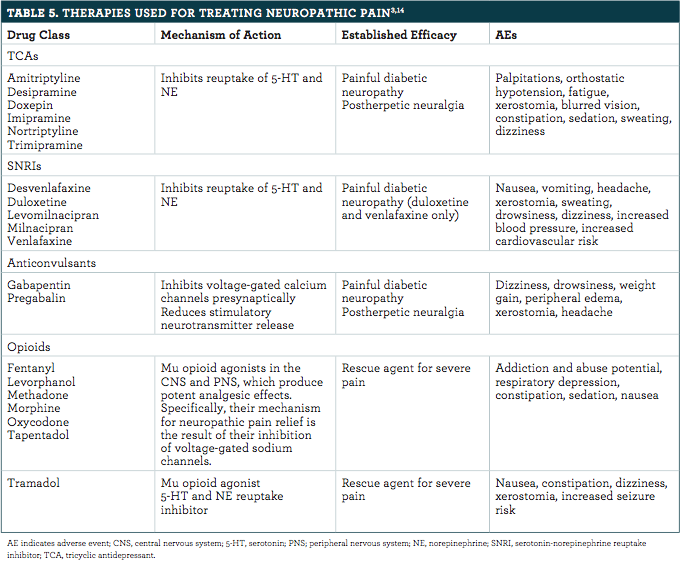
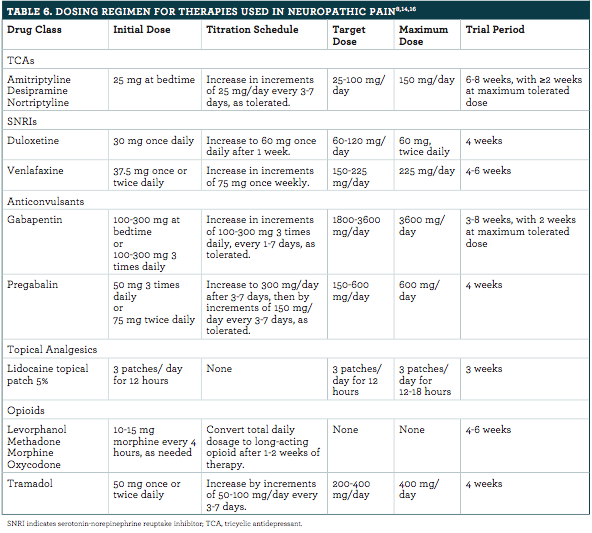
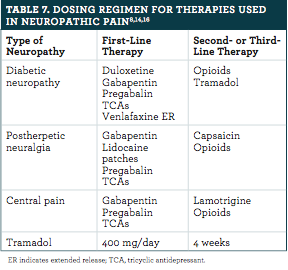
The main drug classes used are antidepressants, anticonvulsants, and opioids. Tricyclic antidepressants (TCAs) have many AEs because they bind to other receptors, such as alpha-adrenergic, histaminergic, and muscarinic.14 Patients tend to tolerate desipramine better than amitriptyline. However, there are not enough data to support the use of desipramine in diabetic neuropathy.8,15 Serotonin-norepinephrine reuptake inhibitors have fewer AEs compared with TCAs because of their higher specificity to binding sites.14 Gabapentin and pregabalin have a similar mechanism of action, but pregabalin has more stable pharmacokinetics.8 Other anticonvulsants are available as alternative options (carbamazepine, oxcarbazepine, and topiramate). However, these agents are generally not recommended and should not be used unless patients are being managed by a specialist. Notably, carbamazepine is for the first-line treatment of trigeminal neuralgia, for which typical doses are 200 to 400 mg twice daily.7,8 The recommended first-, second-, and third-line therapies are outlined in online table 7.3,16
ROLE OF THE HEALTH CARE PROVIDER
Health care providers play a pivotal role in the management of neuropathic pain, from diagnosis to drug therapy. They are responsible for identifying the cause, establishing patient goals, developing an appropriate treatment plan, and assessing a patient’s well-being. In addition to physical pain, there is a significant emotional burden that accompanies neuropathy. Studies have shown that neuropathic pain negatively affects patients’ quality of life, physical functioning, and emotional well-being.14 During a public meeting held by the FDA in 2016, individuals X living with chronic neuropathic pain shared their perspectives about the disorder. Neuropathic pain constantly disrupted their sleep and affected their careers and relationships.17 Patients also seemed more prone to worry about the future.17 Slowly losing the ability to function takes a toll on patients daily, both physically and emotionally. To decrease physical pain and improve quality of life, the source of pain must be identified, multimodal treatment should be used, and emotional support must be given.
CONCLUSION
Neuropathic pain is a multifaceted disease requiring multimodal treatment. With patients’ symptoms ranging from mild discomfort to intense unabating pain, health care providers must balance their patients’ emotional and physical needs with effective drug therapy. Successful treatment requires individualized treatment plans, with the use of anticonvulsants, antidepressants, and other pharmacological therapies. The role of the provider will be as both a medication prescriber and an empathic discerner of the patient’s priority of treatment needs to improve quality of life.
Jerry A. Barbee Jr, PharmD, BCPS, CPh, and Matthew Savoie, PharmD, are clinical hospital pharmacists in Pensacola, Florida.
Catherine M. Kew is a PharmD candidate at Auburn University in Alabama.
Alexis Smith is a PharmD candidate at the University of Maryland Eastern Shore in Princess Anne.
References
DiBonaventura MD, Sadosky A, Concialdi K, et al. The prevalence of probable neuropathic pain in the US: results from a multimodal general-population health survey. J Pain Res. 2017;10:2525-2538. doi: 10.2147/JPR.S127014.
Peripheral neuropathy fact sheet. National Institute of Neurologcal Disorders and Stroke website. ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet. Published December 2014. Accessed December 13, 2017.
Finnerup N, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162-173. doi: 10.1016/S1474-4422(14)70251-0.
Rubin M. Polyneuropathy. Merck Manual Professional Version website. merckmanuals.com/professional/neurologic-disorders/peripheral-nervous-system-and-motor-unit-disorders/polyneuropathy. Updated September 2016. Accessed December 13, 2017.
Rutkove SB. Overview of polyneuropathy. UpToDate. uptodate.com/contents/overview-of-polyneuropathy. Updated September 29, 2017. Accessed December 13, 2017.
Guillain–Barré syndrome. World Health Organization website. who.int/mediacentre/factsheets/guillain-barre-syndrome/en/. Updated October 2016. Accessed December 13, 2017.
National Institute for Health and Care Excellence. Neuropathic pain – pharmacological management. https://www. nice.org.uk/guidance/cg173/evidence/neuropathic-pain-pharmacological-management-full-guideline-191621341. Updated February 2017. Accessed December 13, 2017.
Markman J, Narasimhan SK. Neuropathic pain. Merck Manual Professional Version website. merckmanuals.com/professional/neurologic-disorders/pain/neuropathic-pain. Updated April 2014. Accessed December 1, 2017.
About peripheral nerve disorders. ColumbiaDoctors, Neurological Surgery website. columbianeurosurgery.org/conditions/peripheral-nerve-disorders/. Accessed December 13, 2017.
Autonomic neuropathy. MedlinePlus website. medlineplus.gov/ency/article/000776.htm. Updated December 5, 2017. Accessed December 13, 2017.
Svokos K. The pathophysiology of neuropathic pain. Practical Pain Management website. practicalpainmanagement.com/pain/neuropathic/pathophysiology-neuropathic-pain. Updated December 29, 2011. Accessed December 13, 2017.
Toxic neuropathy. Foundation for Peripheral Neuropathy website. foundationforpn.org/what-is-peripheral-neuropathy/causes/toxins/. Accessed December 13, 2017.
Swenson R, Cohen J, Fadul C, Jenkyn L, Ward T. Disorders of the Nervous System. dartmouth.edu/~dons/part_2/chapter_19.html. Published 2008. Accessed December 13, 2017.
Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(suppl 3):S3-S14. doi: 10.4065/mcp.2009.0649.
Fudin J, Bettinger J, Wegrzyn E. Treatment of neuropathic pain. Pharm Times®. pharmacytimes.com/publications/health-system-edition/2017/march2017/treatment-of-neuropathic-pain. Published April 16, 2017. Accessed December 13, 2017.
Bril V, England J, Franklin GM, et al. Evidence-based guideline: treatment of painful diabetic neuropathy: report of the American Academy of Neurology, the American Association of Neuromuscular and Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2011;76(20):1758-1765. doi: 10.1212/WNL.0b013e3182166ebe.
FDA. The voice of the patient. https://www. fda.gov/downloads/ForIndustry/UserFees/PrescriptionDrugUserFee/UCM542169.pdf. Published February 2017. Accessed December 13, 2017.
http://www.pharmacytimes.com/publications/health-system-edition/2018/march2018/neuropathic-pain-a-glimpse-inside-the-unabating-affliction

No comments:
Post a Comment
All comments welcome but advertising your own service or product will unfortunately result in your comment not being published.