Foot Ulcers
Medically reviewed on Feb 19, 2018
Health Guide
What Is It?
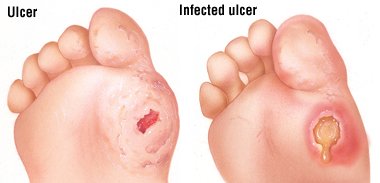
A foot ulcer is an open sore on the foot.
A foot ulcer can be a shallow red crater that involves only the surface skin. A foot ulcer also can be very deep. A deep foot ulcer may be a crater that extends through the full thickness of the skin. It may involve tendons, bones and other deep structures.
People with diabetes and people with poor circulation are more likely to develop foot ulcers. It can be difficult to heal a foot ulcer. In people with these conditions, even a small foot ulcer can become infected if it does not heal quickly.
If an infection occurs in an ulcer and is not treated right away, it can develop into:
An abscess (a pocket of pus)
A spreading infection of the skin and underlying fat (cellulitis)
A bone infection (osteomyelitis)
Gangrene. Gangrene is an area of dead, darkened body tissue caused by poor blood flow.
Among people with diabetes, most severe foot infections that ultimately require some part of the toe, foot or lower leg to be amputated start as a foot ulcer.
Foot ulcers are especially common in people who have one or more of the following health problems:
Peripheral neuropathy. This is nerve damage in the feet or lower legs. Diabetes is the most common cause of peripheral neuropathy. When nerves in the feet are damaged, they can no longer warn about pain or discomfort. When this happens, tight-fitting shoes can trigger a foot ulcer by rubbing on a part of the foot that has become numb.
People with peripheral neuropathy may not be able to feel when they've stepped on something sharp or when they have an irritating pebble in their shoes. They can injure their feet significantly and never know it, unless they examine their feet routinely for injury.
Many elderly people and diabetics with vision problems also can't see their feet well enough to examine them for problems.
Circulatory problems. Any illness that decreases circulation to the feet can cause foot ulcers. Less blood reaches the feet, which deprives cells of oxygen. This makes the skin more vulnerable to injury. And it slows the foot's ability to heal.
Poor circulation in the leg arteries is called peripheral artery disease. It also causes pain in the leg or buttock during walking. It is caused by atherosclerosis. This is a disease in which fatty deposits of cholesterol build up inside arteries.
Abnormalities in the bones or muscles of the feet. Any condition that distorts the normal anatomy of the foot can lead to foot ulcers. This is particularly true if the foot is forced into shoes that don't fit the foot's altered shape. Examples are claw feet, feet with fractures, and cases of severe arthritis.
More than any other group, people with diabetes have a particularly high risk of developing foot ulcers. This is because the long-term complications of diabetes often include neuropathy and circulatory problems. Without prompt and proper treatment, a foot ulcer may require hospital treatment. Or, it may lead to deep infection or gangrene and amputation.
In addition to diabetes, other medical conditions that increase the risk of foot ulcers include:
Atherosclerosis. This condition involves poor circulation to the legs.
Raynaud's phenomenon. This condition causes sudden episodes of decreased blood flow to the fingers and toes. During these episodes, the fingers and toes turn white as the blood supply diminishes. They turn blue, and red again as the circulation returns to normal.
It is rare for a foot ulcer to be unrelated to these risk factors and illnesses. A foot ulcer in a person who has none of these health problems may need to be checked for skin cancer, especially squamous cell carcinoma. This cancer occasionally looks like a foot ulcer.
Symptoms
A foot ulcer looks like a red crater in the skin. Most foot ulcers are located on the side or bottom of the foot or on the top or tip of a toe. This round crater can be surrounded by a border of thickened, callused skin. This border may develop over time. In very severe ulcers, the red crater may be deep enough to expose tendons or bones.
If the nerves in the foot are functioning normally, then the ulcer will be painful. If not, then a person with a foot ulcer may not know it is there, particularly if the ulcer is located on a less obvious portion of the foot.
In disabled or elderly patients, a relative or caregiver may be the one who becomes aware of the problem. The caregiver may notice that foot looks red and swollen. There may be drainage on the sock and a foul odor.
Diagnosis
In most cases, your doctor can tell that you have a foot ulcer simply by looking at your foot.
If you have diabetes, your doctor will assess your control of your blood sugar. He or she will ask about the care that you take to keep your feet healthy. The doctor will ask about the type of shoes that you usually wear.
Your doctor will evaluate the ulcer to determine:
How deep the ulcer is
Whether there is an infection
Whether that infection has developed into cellulitis (a deep skin infection) or osteomyelitis (an infection of the bone near the ulcer)
Whether you have any foot abnormalities, circulatory problems or neuropathy that will interfere with healing.
Your doctor may ask you to walk as part of your examination. This is because your gait may highlight knee and ankle abnormalities that cause abnormal pressure spots on the feet. Your doctor also will look for other foot problems, such as claw foot or fallen arches.
To check for neuropathy, your doctor may:
Test the sensation in your feet
Check your reflexes
Use a tuning fork to see if you can feel the vibration in your toes
Your doctor also can test the circulation in your legs and feet. He or she can do this by feeling your pulses and noting whether your feet are pink and warm. If your pulses are weakened, then your doctor may use Doppler ultrasound to test your circulation.
Your doctor may use a cotton swab or other thin probe to examine the ulcer itself. These tools can be used to see how deep the ulcer is. And they can help check for exposed tendons or bones. Your doctor will look closely for redness around the ulcer. A large margin of redness can be a sign of cellulitis.
Your doctor may order other tests to better understand the extent of the ulcer and to determine whether it is infected. These tests may include:
Blood tests
Bacterial cultures of the ulcer
X-rays
Magnetic resonance imaging (MRI)
A computed tomography (CT) scan
A bone scan
Expected Duration
How long a foot ulcer lasts depends on:
The depth of the ulcer
Whether there is enough blood circulation to supply oxygen and nutrients
Whether the ulcer can be protected from rubbing or pressure
Whether the ulcer is infected
In people who have good circulation and good medical care, an ulcer sometimes can heal in as few as three to six weeks. Deeper ulcers may take 12 to 20 weeks. They sometimes require surgery.
Prevention
People who are at risk of foot ulcers, such as those with diabetes, can take steps to help prevent foot ulcers. They can do this by examining their feet routinely and following good foot-hygiene practices.
The following strategies may help prevent foot ulcers:
Examine every part of your feet every day to check for rubbed areas, cracks or calluses. If necessary, use a mirror to check the heel and sole. If your vision is not good, ask a relative or caregiver to examine your foot for you.
Practice good foot hygiene. Wash your feet every day using mild soap and warm water. Dry thoroughly, especially between the toes. Apply moisturizing lotion to dry areas, but not between the toes.
Wear shoes that fit well and soft, absorbent socks. Always check your shoes for foreign objects and rough areas before you put them on. Change your socks immediately if they become wet or sweaty.
Trim your toenails straight across with a nail clipper or emery board.
If you have corns or calluses, ask your doctor about how to care for them. Your doctor may determine that these problems are best treated in his or her office rather than at home.
Treatment
If you have good circulation in your foot, your doctor may treat your foot ulcer with a procedure called debridement. This consists of trimming away diseased tissue. He or she also will remove any nearby callused skin.
The doctor then will apply a dressing. He or she may prescribe specialized footwear to relieve pressure on the ulcerated area. This specialized footwear may be a cast. Or it may be a loosely fitting postoperative walking shoe or sandal that can be worn over a bandage.
Your doctor will need to see you frequently to examine and debride the area. A nurse may need to visit you to change the dressing every several days. Care of a foot ulcer can require multiple visits over weeks or months. The visits will last for as long as it takes for your ulcer to heal completely. If there is a possibility of infection, you may be given antibiotics.
Once the ulcer has healed, your doctor may prescribe roomy, well-cushioned footwear. This footwear should not put pressure on vulnerable areas of your feet. This will help to prevent ulcers in the future.
Foot ulcers that do not respond to more conservative therapy may require surgery. In certain situations, without leg surgery, the ulcer may not heal properly.
People with poor circulation may need a procedure or surgery to open one or more blocked arteries in the legs. When possible, doctors will try to open the blockage with angioplasty. This is usually done by threading a deflated balloon with a wire mesh cover (called a stent) into the blocked area. The balloon is inflated. This opens the artery. The stent stays in place to hold the artery open. For more significant blood flow problems, surgery is usually needed to re-route blood flow through the leg using a bypass artery.
When To Call a Professional
If you have diabetes, poor circulation or peripheral neuropathy, examine your feet every day.
Call your doctor promptly if you see an area of:
Redness
Swelling
Bleeding
Blisters
Also call if you see any other problem on the foot surface.
Prognosis
When foot ulcers are not deep, the outlook for healing is good if circulation to the foot is adequate. With the best wound-care methods available, most ulcers heal within 12 weeks.
However, about one in three healed ulcers return. This is most likely in people who do not wear specialized footwear prescribed by their doctors.
https://www.drugs.com/health-guide/foot-ulcers.html

No comments:
Post a Comment
All comments welcome but advertising your own service or product will unfortunately result in your comment not being published.